Introduction
Discrimination in healthcare is a reality that minority populations worldwide face every day. However, many people do not realize just how much this bias affects medical care until people find themselves in the waiting room at an appointment or on the receiving end of what appears to be less-than-stellar treatment. In this blog post, we will take a look into institutional discrimination and its implications in healthcare environments across different countries and cultures, exploring patterns of bias against certain social groups as well as signs that such discriminatory practices are leaving individuals feeling like they have to fight harder for their basic rights when it comes to seeking medical attention based solely on their identity. By highlighting real-world examples and analyzing data collected through research studies, we can open up a conversation about the inequalities present in society today and strive for better outcomes for all individuals, regardless of who they are.
Factors Contributing to Racial and Ethnic Disparities Within the Healthcare System
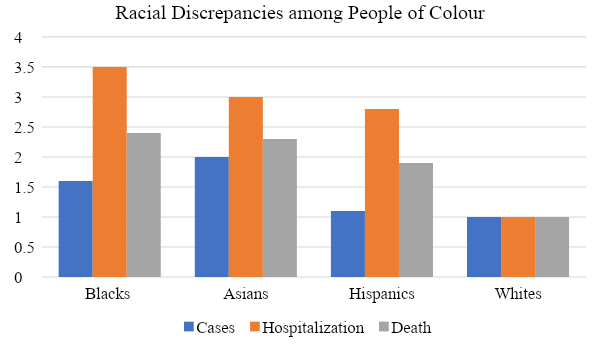
Racial and ethnic disparities in healthcare are a major public health problem, as evidenced by multiple studies showing that certain minority populations receive less access to quality healthcare than their white counterparts. These factors involve access to resources, communication barriers between providers and patients, unequal distribution of services within communities, and discriminatory practices within healthcare institutions. Studies conducted by the National Institutes of Health purport unequal distribution of services between minority and non-minority populations (Health Disparities and Health Equity, 2020). These disparities include access to care, the percentages of uninsured individuals, differences in diagnosis and treatment decisions, and lower use of preventive health services. This is due to economic barriers that restrict access to healthcare services, such as lack of health insurance and poverty populations (Health Disparities & Health Equity, 2020). Furthermore, these disparities are caused by cultural and linguistic differences between minority and non-minority populations and discriminatory practices in healthcare institutions due to implicit bias or racism.
Public policies have also contributed to racial and ethnic disparities in healthcare. For example, the Affordable Care Act (ACA) implemented numerous reforms to the US healthcare system, such as introducing subsidies and expanding Medicaid coverage (Affordable care act). However, in some states that did not expand Medicaid under the ACA, disparities between minorities and non-minorities have grown larger (Orgera & Garfield, 2021). In addition, inequitable access to care is caused by geographic barriers and lack of transportation, further exacerbated by policies restricting care in rural areas.
Overall, racial and ethnic disparities in healthcare can have serious consequences for minority populations. These disparities must be addressed through public policy reforms and an increased focus on eliminating discriminatory practices within healthcare institutions. With these changes, we can work towards improving access to quality health care and addressing the underlying causes of these disparities.
Assessment of the Impact of Racial Disparities on Other Areas in the Life of Minorities
In addition to disparities in healthcare access, minorities also face a disproportionate burden of negative economic outcomes resulting from racial discrimination and inequality. A study published by the National Bureau of Economic Research found that blacks were more likely to experience unemployment during the 2007–09 recession than their white counterparts (Cusick et al., 2022). Another area where minorities are disproportionately impacted is education. Data from the National Center for Education Statistics show that African American students are less likely to complete high school by age 19 than white students; only 74% of African Americans met this benchmark in 2016 compared to 89% of whites (Brey, 2019). This disparity is particularly striking among African-American males; only 68% of African-American males completed high school on time, as opposed to 82% of white males (Brey, 2019). These disparities in educational attainment and employment directly affect healthcare access, as minorities often lack necessary medical care and preventive services that can help them stay healthy enough to pursue educational opportunities or maintain stable employment.
To combat these racial disparities, public policies must be implemented at the institutional level to ensure equitable access to healthcare services for all individuals, regardless of race. For example, the Affordable Care Act was designed to expand healthcare coverage and access to millions of Americans, including minorities (Crowley & Bornstein, 2019). The ACA has successfully reduced uninsured rates among African Americans and other minorities; even with the changes made by the current administration, the uninsured rate remains at a historic low of 11% (How the Affordable Care Act Has Narrowed Racial and ethnic disparities in Access to health care, 2020). By increasing access to healthcare and improving preventive services, public policies can help reduce educational attainment and employment disparities and ultimately improve economic outcomes for minority populations. Investing in equitable healthcare is essential for creating an inclusive society where all people can live healthier lives and have a chance at success.
Ways Public Policies are Linked to Racial and Ethnic Disparities within the Healthcare System
Public policies in the United States, including those related to healthcare, have profoundly impacted racial and ethnic health disparities. These disparities arise from multiple factors, such as unequal access to resources, structural racism, and unequal treatment within the healthcare system. To address these disparities and move toward more equitable outcomes for all patients, it is important to understand the various public policies that have contributed to them.
One example of a policy contributing to racial and ethnic disparities in healthcare is Medicare’s risk adjustment formula, which reduces payment rates for providers based on patient demographics such as race and ethnicity. This has resulted in lower reimbursement rates for hospitals caring for minority patients, leading to poorer quality care and worse outcomes for these patients. Furthermore, research has found that Medicare’s risk adjustment formula is more likely to underestimate the resources required for minority patients than for white patients, resulting in even greater disparities in care.
Another example of a policy that contributes to healthcare disparities is the lack of access to health insurance in minority communities. Many minority groups are more likely to be unemployed and unable or unwilling to purchase private health insurance due to its cost. This can lead to delays in seeking medical care and poorer outcomes overall, particularly for chronic illnesses requiring ongoing monitoring and care. Structural racism and implicit bias can also play a role in contributing to healthcare disparities. Studies have found that when individuals of color experience implicit bias in the healthcare setting, it leads to poorer quality care and decreased patient satisfaction. This can result in worse health outcomes for these patients.
Another factor contributing to racial and ethnic disparities in healthcare is poverty-related policies such as Medicaid funding restrictions. When Medicaid funds are limited, it restricts access to care and increases costs for lower-income individuals who may be disproportionately people of color. Additionally, many states have passed legislation limiting the ability of low-income patients to access health insurance coverage under Medicaid or other subsidized plans, resulting in poorer health outcomes for minorities.
Discriminatory practices within the healthcare system can result in unequal care for patients of color. Studies have found that physicians often use racial stereotyping when making clinical decisions, resulting in more negative outcomes for people of color (Park et al., 2021). Additionally, these practices may lead to lower rates of preventive care and follow-up treatment for minority patients, further exacerbating health disparities.
Policy Strategies for Reducing Discrimination Healthcare Institution
Discrimination in healthcare institutions is a pervasive problem identified and documented through numerous studies. However, reducing institutional discrimination is difficult as it addresses underlying unequal power dynamics, privilege, and access to resources. One policy strategy for reducing institutional discrimination is to promote diversity in healthcare institutions (Togioka et al., 2022). This can be achieved by creating job opportunities for individuals from minority backgrounds, increasing the representation of minorities in decision-making roles, and providing cultural competence training for staff members (Togioka et al., 2022). Additionally, healthcare institutions should create policies that provide financial incentives to those who practice cultural sensitivity and that penalize those who engage in discriminatory activities.
Another policy strategy for reducing institutional discrimination is to create systems of accountability. This can be done by creating a complaint system where individuals can report incidents of discrimination, establishing an independent review board to investigate complaints, and holding healthcare institutions accountable through fines or other penalties for violations (Hassen et al., 2021). Additionally, healthcare institutions should train staff members to recognize and respond appropriately to incidents of discrimination.
Policy strategies alone will not be enough to reduce institutional discrimination. It is also essential that healthcare institutions implement measures that foster an open and supportive environment where all individuals are respected and treated equally. This can be done by implementing anti-discrimination policies and providing cultural sensitivity training for staff members (Togioka et al., 2022). Additionally, healthcare institutions should ensure that all individuals have access to quality care regardless of race, ethnicity, gender identity, or sexual orientation.
Ultimately, reducing institutional discrimination will require a comprehensive approach tailored to each context’s unique needs and supported by strong accountability systems. By implementing evidence-based policy strategies and creating an open and supportive environment, healthcare institutions can reduce racial disparities in access to quality care.
Conclusion
Despite the implementation of numerous changes to healthcare over the past few decades, racial discrepancies remain an ever-present issue in America. Minorities have been shown to receive worse quality care than their Caucasian counterparts, and this reality has devastating consequences. The life expectancy for ethnic communities is shorter, and their chronic disease rate is higher, proving that more must be done to fix this problem. This blog post aims to increase awareness of these disparities and work toward solutions that help provide equal access to quality healthcare for all patients, regardless of race.
References
Affordable care act. (n.d.). Affordable care act (ACA). Glossary | HealthCare.gov. Web.
Brey, C. de. (2019). Status and trends in the education of racial and ethnic groups 2018. National Center for Education Statistics (NCES) Home Page, a part of the US Department of Education. Web.
Crowley, R. A., & Bornstein, S. S. (2019). Improving the patient protection and affordable care act’s insurance coverage provisions: A position paper from the American College of Physicians. Annals of Internal Medicine, 170(9), 651. Web.
Cusick, J. V., Coleman, M. A., Shepherd Director, M., Lofgren, E. A., Gordon, P., Parshall, J. S., Khattar, R., Roque, L., Mirza, Z., Glass, A., Buchanan, M. J., & Banks, L. (2022). On the persistence of the black-white unemployment gap. Center for American Progress. Web.
Hassen, N., Lofters, A., Michael, S., Mall, A., Pinto, A. D., & Rackal, J. (2021). Implementing anti-racism interventions in healthcare settings: A scoping review. International Journal of Environmental Research and Public Health, 18(6), 2993. Web.
Health Disparities and Health Equity. (2020). Health Disparities and Health Equity. National Institute of Neurological Disorders and Stroke. Web.
How the affordable care act has narrowed racial and ethnic disparities in access to health care. (2020). How the affordable care act has narrowed racial and ethnic disparities in access to health care. How ACA Narrowed Racial-Ethnic Disparities Access to Health Care | Commonwealth Fund. Web.
Orgera, K., & Garfield, R. (2021). The coverage gap: Uninsured poor adults in states that do not expand Medicaid. KFF. Web.
Park, J., Saha, S., Chee, B., Taylor, J., & Beach, M. C. (2021). Physician use of stigmatizing language in patient medical records. JAMA Network Open, 4(7). Web.
Togioka, B. M., Duvivier, D., & Young, E. (2022). Diversity and discrimination in healthcare – NCBI bookshelf. National Library of Medicine. Web.
