Introduction
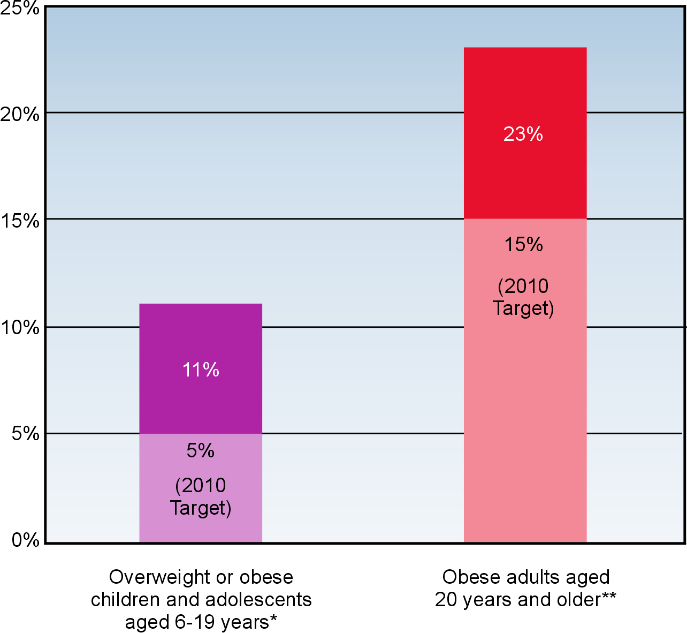
Overweight and obesity are leading health indicators in USA (Figure 1). Studies have revealed that over two-thirds of American adults are considered to be overweight and nearly one-third of the children and the adolescents are obese. Children being overweight are likely to remain obese at adult stage. The prevalence of obesity among children and adolescents have doubled in numbers since 1970 (Wang, 2000).
Obesity is a risk for many fatal diseases—i.e., diabetes, arthritis, cerebrovascular accidents, malignancies. An anti-obesity program can be a feasible solution to the problem at hand. In order to develop a program that is sustainable with desirable results, a logic model can be used. The brief aims to develop an anti-obesity program using a logic model.
Logic Models
The logic model is a linkage developed to ascertain the performance of a program where it includes the evaluation of a program and a sensible representation in the way the program works. According to Wholey et al. (1987), the elements of logical model are resources, activities, outputs, customers reached, the relevant external influences and outcomes—short, intermediate or longer term (McLaughlin Jordan, 1998). Typically, the term logic model is often used interchangeably with the program theory in the evaluation field. It should be noted that logic models can be termed as theory because they describe how a program works and the level of program output (Foundation, 2004).
To ensure effective planning and success of a program, a logic model is used in program because it is known to provide positive results. The logic models have also been described as a systematic and visual representation of the resources, activities and proposed program. Practical examples have revealed that putting logic models in its orderly manner yield the desired results (Wells & Banning, 2008).
The logic model gives clear pictures of how an organization does its short term and long term goal in order to achieve its objectives. The development of logical models and its evaluation provide an orientation to the underlying principles and language of the program planning, implementation and dissemination of results. It should be noted that a good evaluation reflects clear thinking and responsible program management. Logical model enhances the participatory role and is an important step in building community capacity and strengthening community voice. It is also an anticipation to build a clear map for a program (Foundation, 2004).
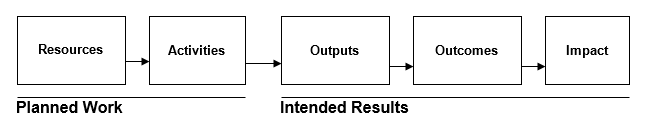
Figure 2 illustrates a basic logic program where it shows the linkages between a planned program and its intended results. The logic models provide the stakeholders a road map and the need to plan a program to achieve a desired result. By mapping a proposed program, there will be visualization and understanding of contribution of human and financial investments for the achievement of the intended program goals (Foundation, 2004). The program of the logic models are as follows:
- Resources Input: These are the inputs that include human, financial, organizational and community resources that need to be directed toward a certain program. These resources are normally used for the operation of a program and are sometimes called inputs. (Foundation, 2004)
- Program Activities: Having access to these resources input enhance the stakeholder to direct them towards a program activities. These are the processes, tools, events and technology that are intentionally used for the implementation of the program. These activities bring out the output of the program. (Foundation, 2004)
- Outputs: The accomplishment of the planned activities bring about the output that will be delivered for a certain program and this will lead to output of the intended amount of service. The direct program activities may include target of services delivered for a program. (Foundation, 2004)
- Outcomes: The outcomes of a program reflect the extent of how planned activities are achieved. The results bring the outcomes of a program, which bring out its benefits. It should be noted that with proper implementation of a program, there should be attainable short term outcomes within 1 to 3 years and the long term outcomes should be achieved within 4 to 6 years. The short-term and long-term outcomes should also be reflected within 7 to 10 years. (Foundation, 2004)
- Impact: The impact is the benefits of the logic models are achieved. The impact brings about some certain changes in the communities and among the target population. Meanwhile, this is fundamental intended changes and this must be achieved within 7 years of implementation of a program. (Foundation, 2004)
The Incidence of Obesity in New Jersey
A research conducted by Wang (2000) revealed an increase in the 15 percent of the obesity cases between 1971 and 1974. The epidemic of obesity has been recognized to be associated with the increase in disease morbidity and even mortality—increasing incidences of patients with hypertension, diabetes, cardiovascular disease, gallbladder disease and some type of cancers. In addition, the occurrence of obesity has also been identified to cause psychological dysfunctions on certain people. The global epidemic has been known in both developed and developing countries. Children being overweight are likely to remain obese at adult stage.
The studies have revealed that over two thirds of American adults are considered to be overweight and nearly one-third of the children and the adolescents also have obese bodies. The prevalence of obesity among children and adolescents have doubled in numbers since 1970, while there has been four times the increase in the prevalence of obesity among the adults in the United States.
Obesity occurs in individuals when there is an excess accumulation of fat in the body leading to health problems. An individual is considered to be obese if he or she has body mass index (BMI)—determined by dividing height by kilogram—to be over 30. Meanwhile, a person is considered to be overweight if the BMI is between 25 and 29.9. (Center for Health Statistics, 2006).
In the United States, the epidemic of obesity is known to lead to the complication of certain types of disease and death. In the year 2000, the effective direct and indirect approaches to reduce the obesity epidemic cost the government $117 billion. The money was diverted on the campaign and the publicity to reduce the epidemic of obesity in the United States (Wang, 2000).
Numerous studies have revealed the occurrence of obesity to be caused by the same biological, cultural, environmental and social factors, which affect the energy intake of an individual. The high energy calorie intake and physical inactivity has been known to be the leading factors of obesity. The excessive energy intake has been known to be risky factor obesity. The intake of fats and some dietary composition such as soft drinks and snacks have also been linked to the occurrence of obesity.
Although several studies have revealed that physical inactivity has been the major cause of obesity among the adult in the United States. It has been revealed that nearly half of the adult population in the United States has not been engaging in the physical activity. In addition, bicycling has dropped among the children and youths by 40%. The sedative activities such as playing video games, watching television and using computers have also dramatically increased among youths and these activities are among the factors leading to the obesity in the United States (Wang, 2000).
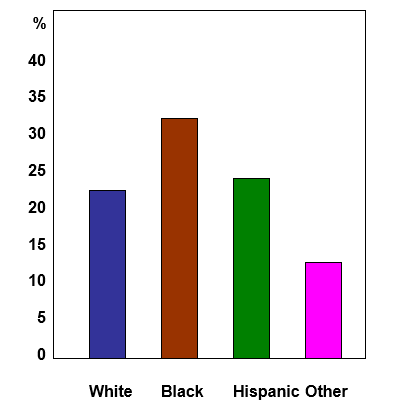
In New Jersey, there has been a consistent rise of obesity since the 1990s. The 2005 health survey revealed that 37% of the New Jersey residents were overweight while 22% were obese, and the rest of 15% of the residents have the risks of becoming overweight. The overall statistics reveal that significant population of New Jersey Black residents are obese, while 22% of Whites and Hispanics were also obese. Moreover, studies also revealed that the people aged between 45 and 64 are considered being obese more than other age group and nearly 55% of the New Jersey population are obese (Center for Health Statistics, 2006).
The high prevalence of obesity in the New Jersey has led the New Jersey government to embark on the New Jersey Obesity Prevention Action Plan. It should be noted that the obesity prevention task force was set aside to address the prevalence of obesity in New Jersey and the Task Force’s intention was to reverse the obesity epidemic in the state (Center for Health Statistics, 2006).
No to Obesity—a Child’s Anti-obesity program
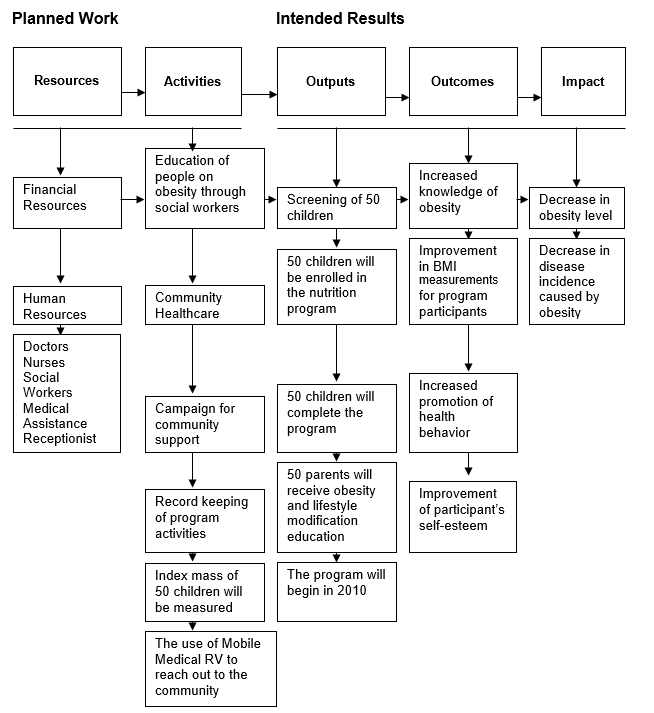
In the feasibility of the program, the analysis and illustrations will be used to show the short-term and long-term commitment required to successfully enable positive change. In carrying out this target, there will be implementation of the logic model and the program will be named “No to Obesity—a Child’s Anti-obesity Program.” The proposed program of “No to Obesity” Clinic for the prevention of obesity is illustrated in Figure 4. A summary of the practical application of the logic models is reviewed in the Table 1.
Resources Input
“No to Obesity—a Child’s Anti-obesity Program” is designed to run for 5 years with hopes for it to be self-sustaining. The program will seek funds. The target fund will be determined at a later date, which will be directed for the use of promotions and advertisements. Time usage of current Doctors and Nurse practitioners to manage the program will be determined in relation to financial feasibility. Staff will be determined in relation to role and ability, i.e., social workers, medical assistants and receptionists.
Program Activities
The company will put program activities into action for the prevention of obesity. The program activities will take place upon availability of financial and human resourcesThe “No to Obesity—a Child’s Anti-obesity program” will be set up in 2010. In the program, the clinic will establish a program manager, providers and clinical support staff who will participate in treating overweight and obese patients. The three main areas of focus for the internal program will be diet/nutrition, exercise and lifestyle behavioral changes. Awareness will also be a main theme to focus on the community aspect of obesity.
The Body Mass Index of 50 obese people, which will consist of 50 children, will be established as the initial program target population. If the computed BMI falls into an overweight or obese category, the child will be selected for the program. There will be a 3-week educational program where social workers will take an active part in educating children and parents alongside the providers and clinical support staff.
In addition, the program will screen the BMI of 100 patients daily. The doctors and nurses will engage in the treatment of the patients towards the reduction of their BMI. This will ensure awareness of all staff and patients about the importance of BMI and that all clients will be receiving screening and education related to obesity regardless of participation in the program. Additionally, social workers with the clinical staff support will engage in parent education so the program will encompass the whole family (Foundation for Community Health, 2007).
The program will seek funding sources which will also assist with the necessary program outreach. Outreach and collaboration with the local hospitals, county department of health, schools, community group and local government for the campaign against obesity will be necessary. The mobile medical RV that the organization owns will be made available for the program and the clinic will use it to reach out to the community and possible patients. Part of the program will be a campaign for community support. The program manager will try to acquire support—which will involve community support as well as cooperation and financial support from business organization. The manager will also engage in the campaign to advise the private and public schools on the prevention of obesity.
In the program, the Program Manager will enhance public awareness for school authorities to provide food guidelines to the students and the nature of the food to eat in maintaining a healthy lifestyle. It is also important that there will be availability of equipments that can improve the physical activities in the school (The State of New Jersey, 2006). In addition, there will be an education program initiative; the goal of this initiative is to reduce both the prevalence and incidence of obesity state-wide and thereby making the chosen town healthier.
Outputs
Outputs will be the accomplishment of the planned activities and the reflection of the program activities on the society. With the implementation of the “No to Obesity—a Child’s Anti-obesity program,” the target is to be aware of the risks of obesity among the people in the community.
In the program, 100 patients per day will be screened for obesity or overweight. A total of 50 children will be enrolled in the full program, which incorporates the staff of the clinic and the child’s family. The program will evolve every 3 weeks with the initiatives of education and promotion of physical activity. Thus, there will also be behavior modification, which may help in the improvement of the children’s lifestyle (New Jersey Primary Care Association, 2008). The outputs of the logic model by the clinic to prevent obesity are: to target to improve more children in participating in physical activity, improved nutritional choices and behavior modification.
Table 1. Summary of practical implementation of basic logic model.
Outcomes
The outcomes of the program for the prevention of obesity have been targeted to provide positive results. Part of the outcomes is that people will become aware that obesity is a disease which can lead to heath complications. There will be increased knowledge of obesity prevention. The program will also help in improving the behavioral attitude of the people. For example, many people will be aware of the importance of physical activity in the reduction of obesity and the body weight along with appropriate nutrition. There should be improvement in BMI measurements for the program participants. Thus, most people will also make effort to embark on physical activity and diet control in order to control their body mass (Department of Health and Human Service, 2008).
Impact
The impact of the program will show a decrease in obesity levels and a decrease in disease due to decreased obesity. The final stage should bring about changes in the community towards the target program and there will be changes in the people’s attitude to attain a healthy life.
Development of an Implementation Evaluation Plan
This section provides the development of an implementation evaluation plan for the “No to Obesity—a Child’s Anti-obesity program.” The evaluation is the cornerstone for the success of this program and its effectiveness lies on a good evaluation. The implementation of the evaluation plan is important because the aspect of the “No to Obesity—a Child’s Anti-obesity program” needs assessments during the formative process of the program. It should be noted that the evaluation plan makes the implementation of the program world-class. Thus, the evaluation of Anto-Obesity Program will make the program objectives achievable coinciding with its predetermined goals (University of Tasmania, 2005).
The implementation of the evaluation is divided into four stages:
- needs assessment and feasibility;
- program design;
- program delivery and
- program improvement.
Stage I. Needs Assessment and Feasibility
The “No to Obesity” Clinic will set up a committee to evaluate the needs assessment and feasibility of the “No to Obesity—a Child’s Anti-obesity program.” The program will be designed so that the campaign for the prevention of obesity will reach all the people in the community. The campaign will run for 5 years and will be evaluated for sustainability. “No to Obesity” Clinic will look for grant sources from the New Jersey’s Department of Health and Senior Services and any other possible grant funding sources. The reason for sourcing for grants will be to initiate and expand the program to other communities and increase resources within the program.
The clinic will engage further the interest of stakeholders in the community to be part of such a program (Cullin et al. 2006). For adequate funding availability on the need for the prevention of obesity in New Jersey, the clinic will evaluate the prevalence of obesity in New Jersey. The evaluation the feasibility of the “No to Obesity—a Child’s Anti-obesity Program” is the milestone for the program and date of the starting of the program will be scheduled for 2010 up to 2015.
Stage II. Plan and Design an Obesity Program in a Primary Care Clinic
The information on the prevalence of obesity in New Jersey necessitates the program design for the “No to Obesity—a Child’s Anti-obesity Program.” While both human and financial resources put forward for the program will be available, the campaign for the program will be designed to make three changes: awareness, lifestyle changes through behavioral modification and long-term changes.
- The program awareness is aimed to increase the level of awareness among people. The methods designed for the improvement of community awareness will be through newsletters, posters, health fairs, radio advertisement and newspaper advertisement. The “No to Obesity” clinic population will be used to initiate the campaign.
- In addition, there will be initiation of learning and skill building, which will be designed for 3 weeks. The aim is to improve the lifestyle change of the people with regard to obesity and the program is designed to have potential impact for the long-term change in BMI.
- Long-term changes will be intended to focus on the lasting behavioral changes and initiating building a lasting weight management behavior among people. This and along with incentives and awards for those families that participate (Minnesota Department of Health, 2008).
Stage III. Program Delivery
The program is aimed to be delivered to the school children and adults who have a BMI that categorizes them as overweight or obese. The program being setup for children and their families will be the main focus. In addition, the program is also designed to be delivered to the private and public practitioners. In the program delivery, the quality assurance process will be put in place to ensure that all the program delivery meets the required standard and this will help to strengthen the delivery of the program. This will also be useful in practice improvement for the other projects.
Stage IV. Program Improvement
In the program improvement, the key partners are to meet on a regular basis to recommend programs that can further promote positive outcomes. The program improvement should also include revision of past policies and promotion of youth and family engagement in the prevention of obesity (Pennsylvania Department of Public Welfare, 2005).
Conclusions
The logic model will be able to demonstrate the importance of sequence planning in the achievement of desired goals. While the logic models have positive importance of providing how an organization works, it also gives a clear understanding on the time to expect the desire result. The total program objective is feasible and attainable.
References
Australian Government. (2009). Development and Implementation of a Program Evaluation Plan for Grain & Grace. Australia: Australian Government.
California Department of Health Services. (2006). California Obesity Prevention Plan: A Vision for Tomorrow, Strategic Actions for Today. Department of Health Services.
Center for Health Statistics. (2006). Obesity in New Jersey. USA: New Jersey Department of Health and Senior Service.
Community Health. (2007). Example of a Logic Model Report Form. USA.
Cullin, A., Giles, T., Rosenthal, J. (2006). Evaluating Community–based Child Health Promotion Programs: A Snapshot of Strategies and Methods. National Academy for State Health Policy.
Department of Health and Human Service. (2008a). Collaborative Areas of Focus: Clinical, Financial, Operational, Health Resource and Service Administration. USA.
Department of Health and Human Service. (2008b). Guide to Physical Activity. National Health Institute.
McLaughlin, J. & Jordan, G.B. (1998). Logic Models: A Tool for Telling Your Program’s Performance Story, Performance Management Network. The Sandia National Laboratories.
Minnesota Department of Health. (2008). Phase Three: Program Design and Implementation. USA.
National Initiatives For Children’s HealthCare Quality. (2007). Expert Committee Recommendations on the Assessment, Prevention and Treatment of Child and Adolescent Overweight and Obesity – 2007 – An Implementation Guide from the Childhood Obesity Action. USA: Utah Government.
National Center for Chronic Disease Prevention and Health Promotion. (2008). Physical Activity and the Health of Young People. National Center for Chronic Disease Prevention and Health Promotion, Division of Adolescent and School Health.
New Jersey Primary Care Association. (2008). What is new in Obesity. Hamilton, New Jersey.
Pennsylvania Department of Public Welfare. (2005). Program Improvement Plan Summary. USA: Commonwealth of Pennsylvania.
The State of New Jersey. (2006). The New Jersey Obesity Prevention Act Plan. USA: The New Jersey Department of Health and Senior Service.
University of Tasmania. (2005). Project Evaluation Toolkit, Center for the Advancement of Learning and Teaching. USA.
Vermont Department of Health. (2006). Preventing Obesity in Vermont: A Statewide Plan Engaging Individuals, Organizations, Communities, Government & Industry. USA: State of Vermont Department of Health.
Wang, Y. (2004). The Obesity Epidemic: Why We Should Be Worried and What we can Do About it? USA: University of Illinois.
Wells, M, S, Arthur-Banning, S, G, (2008), The Logic of Youth Development: Constructing a Logical Model of Youth Development through Sport. Journal of Park and Recreation Administration, 26, 2, 189–202.
Foundation, W.K. (2004). Using Logic Models to Bring Together Planning Evaluation, and Action: Logic Model Development Guide. USA: W.K. Kellogg Foundation.
Wholey, J.S., Hatry, H.P., Newcomer, K.E. (Eds). (2004). Handbook of practical program evaluation, 2nd ed. San Francisco: Jossey–Bass.
