Abstract
Over the years, the world has experienced increasing trends in the dominance and problem of childhood obesity characterised by excess body fats as well as body weighing more than the normal mass considering the ages and heights of the individuals. More specifically, the prevalence of childhood obesity cases has doubled over the last twenty-five years.
The paper tends to explore the prevalence of childhood obesity among children. Further, the study examines the effects of childhood obesity on health as well as recommending the approaches that can aid in solving this complex problem.
Introduction
Child obesity is a global health issue resulting from excess body fats and overweight. Besides, obesity has negative repercussions on the health and wellbeing of children. Also, obesity is currently among the major disturbing health problems. Studies indicate that over 32% of school-going children have developed problems related to an unhealthy increase in body mass.
According to the World Health Organization, obesity is a worldwide pandemic owing to its escalating trends not only in the US but also around the globe. In this regard, several definitions have been advanced to explain obesity. According to the centers for disease control and prevention, obesity results when an individual’s body mass index falls within the range of 25% and above.

Besides, childhood obesity presents many challenges and hazards, ranging from health consequences to psychological difficulties. Moreover, early years of childhood are critical in the development of healthy behaviours and outcomes that determine the future health of an individual.
Currently, the prevalent levels of obesity among children are continuously increasing. Therefore, the problem of overweight is currently a major health issue because of its effects on growth and development in children. As such, it is important to understand the prevalence, causes, associated risk factors, prevention, and intervention measures of childhood obesity.
The Prevalence of Obesity
Obesity arises from a lack of balance between energy consumption and energy expenditure. In England, France, and Korea, there has been a steady augmentation in the number of obese children at a rate of about 7%.
The trends are upsetting among adolescents, thereby initiating an ever-increasing health challenge around the world. Further, according to the World Health Organisation, obesity is responsible for over a million deaths and about 11 million cases related to liver ailments. Overweight exposes individuals to the threats of cardiovascular diseases, diabetes, mental disorders as well as orthopedic concerns. Further, the epidemic can lead to underperformance and low confidence among children.
In modern society, individual energy demands have experienced significant augmenting trends. Various reasons explain the trend, including growth in food output by industries as well as cropping up of a diet consisting of high energy, proteins, and fats. In other words, the alterations experienced in the consumption patterns have come with its problems characterised by the ever-increasing demand for convenient foods that have poor nutritional compositions.
The major concern is the increasing eating of intense energy foodstuffs as well as drinks among the populace. Also, the media continuously play a huge role in carrying out ads that promote the consumption of foods with high levels of fats at the expense of putting more efforts in the promotion of nutritious edibles (Caprio, Daniels, Drewnowski, Kaufman, Palinkas, Rosenbloom & Schwimmer, 2008).
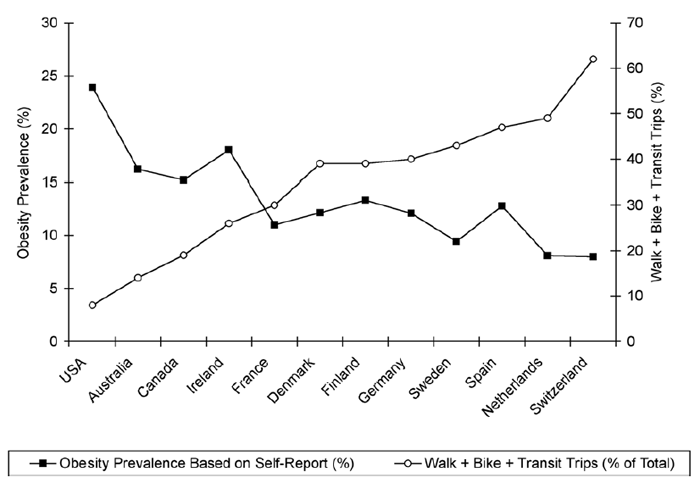
Contemporary society has come up with a diminishing drift in the consumption of energy by promoting the deskbound mode of living. For example, the increase in motorised transport, mechanised equipment as well as labour saving strategies at residences and in schools have brought about the need for exercises leading to the dominance of bodily inactiveness. The lack of physical activity is a major risk concern for the development of other diseases such as premature deaths and cardiovascular arrests.

Obesity increases with color intensity from yellow at 5% to dark red at 45%.
According to the World Health Organisation (WHO), the prevalence of obesity among children based on the body mass indices reflects that Ukraine records the highest rate of about 48%, Greece 17.1%, Spain 35%, Portugal 32%, and France 18% as well as 20% in Sweden among other nations.
Within the category of adolescents, the overweight prevalence among the Irish girls is about 27%, Spanish boys with over 32% and the Czech Republic adolescents exhibit the near to the ground dominance of obesity with about 9%. Most importantly, the data shows that in Canada, there have been augmented tendencies in the proportion of young children having increased overweight as well as the equivalent trend in adults’ obesity at a steady rate of about 4.3%.
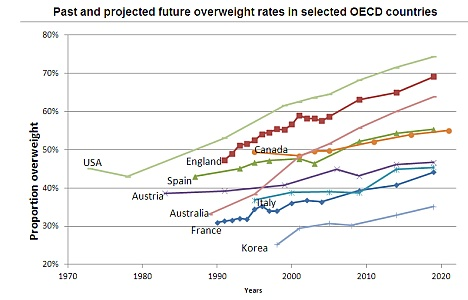
Also, available information exhibits a steady increase in overweight populace from 29% in 1973 to about 42% in 2004. Moreover, the 2007 survey of lifestyle, attitudes, and nutrition exhibits that about 62% of Irish grown-up populace account for overweight. Further, the prevalence of overweight in Eritrea accounts for fewer than 15%. On the other hand, countries such as the United States, New Zealand, and Australia record an obese populace of more than 30%.
Comparing the occurrences of obesity among the developed and developing economies, the incidence of obesity varies from 23% in the Republic of Korea to over 65% in the USA. In developing countries, Indonesia exhibits obese masses of about 73%. According to the findings, it is evident that the dominance of obesity is elevated in the US, followed by the Middle East and Europe. Also, an interesting tendency of obesity has continuously been observed considering age groups.
In this regard, considering the data from the WHO, it is evident that in the first world countries, the majority experience the peak of obesity at advanced adulthood. In contrast, in developing countries, the peak of obesity is experienced in early adulthood. Generally, there has been an increase in obesity rates among children all over the globe.
Causes of Obesity
The prevalence of obesity has continued to pose serious concerns on health matters, making it a global spate. Several factors are to blame for the prevalence of obesity among children.
Culture
Cultures have a greater influence on the child-feeding patterns about the beliefs, attitudes, and behaviours regarding various foods. In other words, Cultural factors that contribute to the increased levels of mass body gain are derived from belief systems of society. For instance, in Kuwait and other Arab countries, women find difficulties taking part in many recreational activities such as active sports and exercises. Also, young girls find difficulties participating in sports or active outdoor exercises, particularly in the presence of men.
The belief system of the society, social stratification also has a profound effect on the health of the. For instance, a review by Caprio et al. (2008) on the influence of race, ethnicity, and cultures on childhood obesity within the US society indicated that the diverse belief systems among the races have a profound effect on childhood obesity.
The study observed that the belief in fast and junky foods among white race has contributed to the increased prevalence rate of obesity among white children. Besides, the belief in lean, low fatty Asian foods has significantly contributed to the decreased prevalence of overweight among the children of Asian origin.
Genetic Factors
Genetic factors contribute hugely to the development of obesity among children. Genetic factors originate from how individual genes influence physiological activities, growth, and adaptation to the environment. Genes determine the functioning of all aspects of human physiology.
Also, genes influence how individuals develop and adapt to the environment. The development of obesity is no exception to genetic control. Also, genes determine how body fats are converted into energy. Moreover, the genetic characteristics influence the way body fats are burnt out while individuals engage in active physical activity.
Gene interactions within the body determine eating habits, appetite control, as well as energy conversions. Essentially, genes that code for leptin hormone resulting from monogenic mutations are closely associated with the development of obesity and overweight. For instance, genetic syndromes resulting from chromosomal abnormalities and gene alterations have also been identified as the major cause of obesity among children.
A twin study conducted by Rampersaud, Mitchell, and Pollin (2008) based on 25 twin pairs and 50 genetic and adoptive family members, suggested that increased body mass has links to genetic factors. Additionally, the fat mass and obesity-associated genes have increased chances (30 to 40%) of causing unhealthy body weight. Another gene that is closely associated with a rear form of monogenic obesity has been discovered within the chromosomes.

Media Advertising
Media advertising, including television, newspapers, radio, and the internet is increasing, thereby influencing the types of lifestyles that people adopt and consequently leading to healthy living habits. Media advertising and an increase in body mass are indirectly related. The rationale is derived from the fact that the increase in media advertising has contributed to health-promotion campaigns that have led to amplified awareness on better eating habits and intake of healthy foods.
A study by Popkin, Adair, and Nig (2012) indicated that mass media provides some form of health-promoting messages, which significantly contribute to decreased levels (11.1%) of obesity and overweight among the male children compared to children devoid of access to media adverts (38.5%).
Family Environment
Parents and families shape the home environment in which children grow. Moreover, parenting styles and family attributes have a greater influence on dietary behaviours and physical activity levels of offspring. Besides, parental body masses are frequently used to predict the possibility of obesity in offspring or later in adulthood.
The reason is not only due to the predisposition of genetic characteristics that parents and children share but also the common attitudes and behaviours that progenies and parents have. A cross-sectional study conducted by Magarey, Daniels, Boulton, and Cockington (2003) on the relationship between parental Body Mass Index (BMI) and children BMI indicates the link between the BMI of the parents and the children. The study indicated that the mothers’ and fathers’ BMIs were significantly but weakly correlated with the children BMI.
The behaviours and the parenting styles have also been hypothesised as influencing the weight statuses of children. However, a study conducted on Australian children between the ages four to five years indicated no correlation between the mothers parenting behaviours and style and the weight gain of the children.
Conversely, the relationship was positive with fathers. For instance, children with more controlling fathers had 26% increases in BMI. Further, other factors such as maternal smoking during pregnancy and enhanced breastfeeding behaviours have also been associated with the risk of being overweight and obese of adult children
Sedentary Lifestyle Factors
Various studies have associated sedentary lifestyles with increased prevalence of obesity and overweight among school-going children. In other words, sedentary life factors have been reported to be the major cause of obesity and overweight among children. El-Bayoumy, Shady, and Lotfy (2009) cross-sectional study indicated that obesity is higher among children leading sedentary lifestyles.
In the study, El-Bayoumy et al. (2009) indicated that obese children spend a lot of time sleeping 8.9 + – 2.3 compared with 8.8 + – 1.2 among normal children. Besides, El-Bayoumy et al. (2009) reported the time spent by school-going children watching TV and playing video games. The report showed that children spending more hours per day are likely to be obese and overweight compared with children spending fewer hours per day.
Lack of Physical Activity
The changes in the socio-economic statuses and the way people live significantly influence the physical activities undertaken by the people. Also, the patterns of outdoor exercises have changed and diminished drastically.
A cross-sectional study by El-Bayoumy et al. (2009) indicated that lack of physical activity has contributed to the increased prevalence of obesity and overweight among the intermediate adolescent school going children of between the ages ten and fourteen. The study indicated that the majority of adolescents of children between the ages of 10 and 14 increased body weights and obesity increased due to physical inactivity.
Dietary Patterns
Dietary patterns also influence the rate at which the bodyweight increases or decreases. According to FAO data, augmented tendency per capita availability of macronutrient calories as well as fats and proteins is evident. For instance, in Malaysia, the intake of calories and fats has been increasing by about 20% over the years. The increase of calories in the body leads to swelling of the body physique.
Further, the macronutrient composition in an individual’s diet also influences body mass. In most cases, the relationship that exists between energy ingestion and the mass depends on the ease of deposition of the surplus macronutrients. Also, the expenses involved in the storage of fats are minimal. In this regard, more fats are stored, thereby increasing the overall weight of the body (Caprio et al., 2008). Excess fat in the body destabilises the equilibrium in the body mass since it is inadequately adjusted at the ingestion and oxidation levels.


Television
Various studies suggest that continuous watching of television s well as playing games is associated with inactivity, which in turn causes unhealthy weight gain. In Kuwait, a study by Armstrong, Lambert, and Lambert (2011) found that the associated risk of being obese was 1.4 for male children between the ages of six to ten spending over four hours watching television compare to 0.72 relative risks of similar male children developing obesity while spending less than four hours watching television.
Armstrong et al. (2011) indicate that about seventeen percent of school-going children between six and sixteen years spend more than two hours watching television. The study also specifies that the proportion of time spent watching television increases with age. The proportion is approximately 0.14 for nine years olds and below while the proportion rises with age to approximately 0.25.

Beverages
Rising consumption of sugary beverages contributes to the increasing prevalence of obesity, particularly among children. Most types of beverages contain over eighty percent sugar that when consumed, contributes to increased calories in the body. Also, children consume higher amounts of beverages per day about other meals contributing to over two-thirds of calories in their daily diets.
Scientific evidence suggests that consuming twenty grams of soda add over 240 calories in the body while sixty-four grams of fountain cola drink would add up to 700 calories in the body. Consuming beverages do not make children full compared with an equal quantity of solid food, yet beverages contain a high amount of calories. As such, there are increased chances of consuming more beverages per day compared with other solid foods.
A study conducted by El-Bayoumy et al. (2009) indicated a rising consumption of sugary beverages, causing increased harm to health. The study indicated that by 2005, children were consuming over 2224 calories per day from beverages adding up to about eighty-nine percent of their daily calorie intake.
Among the children aged between six and eleven years, calories intake from sugary beverages increased by over 60%. Also, the number of children consuming sugary beverages rose by 79%. Further, the study indicated 26% increased risk of developing obesity and overweight related complications among the children and youths consuming sugary beverages.
Effects of Child Obesity
Health and Emotional Problems
The prevalence of obesity has continued to pose serious concerns on health matters, making it a global spate. Obese children often suffer from emotional problems emanating from constant mocking and discrimination by peers and family members. Such forms of stereotyping normally contribute stumpy confidence as well as depression in offspring.
Additionally, lethal conditions, including myocardial infarction, hypertension, as well as sleep difficulties, may result from obesity. Besides, babyhood obesity also results in anorexia and bulimia, along with skin infections. According to the World Health Organisation (WHO) statistics, high intakes of proteins and fats pose the threats of cardiovascular diseases, and renal ailments. Moreover, deep vein thrombosis and complications in surgery and births are health risks associated with overweight (Popkin et al., 2012).
Health Care Costs and Resources
Further, the health care expenses involved in the treatment of child obesity cost billions of dollars annually. Specifically, in the year 2005, close to $200 billion was spent in obesity-related health care outlays. The ever-increasing burden in terms of costs posed by obesity cases has caused great concern across the globe.
More importantly, the management of obesity involves direct costs and indirect outlays. The former refers to the costs that emanate from both inpatient and outpatient health services such as surgery, laboratory and radiological tests as well as drug therapy.
On the other hand, indirect costs are described as the resources that are relinquished in the management of obesity. For instance, the value of lost work and insurance are some of the resources encountered in the management of obesity. For example, days missed by obese children from school are expenses to children since they are unable to catch up with the other normal children. Short-Term absences, long-term disability, and less performance are common features of obese children. Also, remittances of higher life insurance premiums are common for obese children.
The costs and resources involved in the management of obesity-related conditions have shown a steady augmentation of the years. In the US, expenditures on obesity-related conditions represent over 8% of Medicare annually. Theorists argue that if the trend remains unconstrained, the spending on the complex condition is expected to increase further.

Child obesity Intervention Strategies
The complications resulting from childhood obesity are severe. Moreover, there is a likelihood that obesity can continue affecting the child during adulthood. As such, there is a greater need to look into the issue at all levels through the application of actual intermediations and inspirational approaches. Further, there is a need for collaborative efforts from various government agencies, schools, families, and health professionals to provide measures that enhance prevention, control, and management of obesity among children.

Government-based Approach
Governments have full responsibilities of providing measures that promote healthy environments, nutrition as well as other processes that reduce the prevalence of obesity among children (Popkin et al., 2012). Essentially, recognising the most effective and efficient intervention approaches directed towards the enhancement of physical activities as well as providing nutritious diets in schools to reduce the prevalence of obesity children is significant.
As such, governments are obliged to encourage evidence-based programs aimed at improving physical activities and providing healthy foods to children. For instance, in the US, the government has ensured a healthy environment both in school and at the family levels through encouraging evidence-based programs. Besides, the government can contribute positively to the prevention of obesity through policy interventions that educate the public on the possible effects of obesity.
Studies on the effects of implementing legislative school policy in Arkansas indicate that government programs on school meals should be directed towards promoting a healthy environment and nutrition, which in turn lead to the reduction of obesity among children.
Moreover, other studies suggest that physical intervention strategies should be included in the school curriculum. Further, increased obligations of governments in instigating strategies that support and build up healthy environments such as enabling access to healthy and fresh green foods, building walk and bike paths as well as playgrounds on underserved community schools are significant.
Most administration stratagems should be aimed at normalising food production and intake in schools. Essentially, governments’ dealings geared towards reducing and preventing childhood obesity should focus on restrictions and immediate interventions such as instructing food vendors and manufacturers to give accurate caloric comprehensible markers on all food products.
Also, the food vendors and manufacturers should be required to reveal honest calorie contents on food menus. Further, governments should increase their roles by putting limitations on the advertisement of unhealthy foods. Besides, governments should promote healthy food making among parents.
Family-based Approach
Family ties are also one of the structures in which offspring are brought up, and better behaviours are imparted (Magarey et al., 2003). Besides, the parents and family relations have greater influences on the children’s behaviours, including eating habits and lifestyles. As such, the interventions to reduce obesity due to unacceptable eating habits at family echelons are necessary. In other words, effective interventions at the level of the family are of greater benefits to children’s change of overeating and morbid selection of food behaviours.
Essentially, families should be the first to intervene on risks factors related to the increase in children weight through appropriate measures.
For instance, parents can take certain actions that promote physical activities, including encouraging children to walk instead of using family cars as well as utilising the stairs instead of elevators. Family interventions are the most effective means through which obesity can be prevented and reduced among children. Also, family-based weight-control involvement is essential in the reduction of overweight cases among offspring.
In principle, providing good support to parents is a critical strategy. Moreover, mothers have a greater influence on their children (Magarey et al., 2003). As such, family interventions targeting mothers are better strategies in controlling and management of childhood obesity. Parents, families, and peers have a greater influence on eating behaviours of children. Essentially, family interventions focusing on nutrition and dietary behaviours have a greater influence on the management and reduction of childhood obesity.
School-based Approach
Children spend over ninety percent of their time in learning institutions. As such, schools are critical in shaping the behavioural development of the child, particularly eating habits and food choices. Moreover, the schools have the capabilities of monitoring the eating behaviours as well as the food choices of children. Also, schools have abilities in devising various interventions that directly prevent the prevalence of obesity among children. Besides, most interventions have been devised to focus on child nutrition and physical activity.
Studies designate that offspring consume no less than a single repast at school. As such, learning institutions have significant obligations aimed at educating children on the right choices of food. Learning institutions have been at the forefront in manipulating the intake of beverages, including carbonated drinks and other sugary foods among school-going children.
Further, inspiring children to consume healthy food substances is a critical function of schools in reducing obesity cases (Rampersaud et al., 2008). Moreover, healthy nutritious food items in the diets of children and stressing on a balanced diet by schools are important interventions that reduce the prevalence of obesity.
Besides, schools can also participate directly in the control of children weight gain through prolonged physical activity to control weight gain among the children. Schools offer numerous prospects that aid in framing plans aimed at controlling and preventing weight gain and obesity through the generation of settings where children eat healthy meals and frequently participate in physical activities.
School Nurse-based Approach
School nurses have increased responsibilities in fighting childhood obesity and other related unhealthy weight gains in schools through the realisation of diverse interventions. In other words, school nurses have increased opportunities in generating an atmosphere where children can live healthy lifestyles (Magarey et al., 2003). Besides, children taking school meals consume over fifty percent of their daily calories in school. Under such circumstances, schools become an ideal situation where healthy food intake behaviours can be promoted.
As such, within school environments, school nurses can play critical roles in educating the school kids on a healthier diet and collaborate with the school administration in ensuring the meals provided meet the required guidelines for nutrition. Also, school nurses have the knowledge and skills that are required in promoting actions supportive in the management of overweight and obesity as well as capable of dealing with the requirements of overweight and obese children in schools.
Further, the school nurses should provide joint initiatives through collaborating with all the stakeholders and other healthcare providers to encourage procedures that give confidence in healthy weight among children. Besides, school nurses have the responsibility of utilising the know-how to aid in the determination of BMI and blood-pressure screening as well as support continuing follow-ups on children and their families.
More specific, discovery, recognition, and timely intervention as well as enlightening the families and other school stakeholders about the issues of childhood obesity and weight gain are significant roles and ways through which school nurses can help in reducing the prevalence of obesity and overweight in children.
Conclusion
Various risk factors explain the prevalence of childhood obesity ranging from dietary patterns to physical activity. The rise of obesity has been blamed on unhealthy dietary practices embraced by different households. For instance, soft drinks and fast foods that contain higher amounts of fat and sugar have increasingly become the darling of a significant number of children since they are accessible within the families. Consequently, the consumption of such foods leads to increased intakes of energy, thereby increasing the risk of being obese.
Besides, obesity has numerous effects on children’s health. Obesity is a major cause of cardiovascular diseases. Therefore, it is critical for governments, families, schools, and health professionals to undertake collaborative actions that are aimed at reducing obesity, particularly on young children.
References
Armstrong, M. E., Lambert, M. I., & Lambert, E. V. (2011). Secular trends in the prevalence of stunting, overweight and obesity among schoolchildren (1994-2004). European Journal of Clinical Nutrition, 65(5), 835-840.
Caprio, S., Daniels, S. R. Drewnowski, A., Kaufman, F. R., Palinkas, L. A., Rosenbloom, A. L., & Schwimmer, J. B. (2008). Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment. Diabetes Care, 31(11), 2211-2219.
El-Bayoumy, I., Shady, I., & Lotfy, H. (2009). Prevalence of obesity among adolescents (10 to 14 Years) in Kuwait. Asia-Pacific Journal of Public Health, 21(2), 153-159.
Magarey, A. M., Daniels, L. A., Boulton, T. J., & Cockington, R. A. (2003). Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord., 27(1), 505–513.
Popkin, B. M., Adair, L. S., & Nig, S. W. (2012). Global nutrition transition and the pandemic of obesity in developing countries. Nutrition Review, 70(1), 3-21.
Rampersaud, E., Mitchell, B. D., & Pollin, T. I. (2008). Physical activity and the association of common FTO gene variants with body mass index and obesity. Arch Intern Med., 168(16), 1791–1797.
